Introduction: New Horizons in Psychopharmacology
In a significant development in the realm of psychopharmacology, the potential of a novel schizophrenia medication, KarXT, has emerged as a beacon of hope for those suffering from Alzheimer’s disease (AD) and associated psychiatric symptoms. This groundbreaking drug, introduced by the American biotech company Karuna Therapeutics, has recently entered clinical trials to evaluate its efficacy not only for schizophrenia but also for alleviating psychosis linked to Alzheimer’s disease, and possibly the symptoms of bipolar disorder.
Revolutionary Mechanism of Action
KarXT stands out as the first schizophrenia medication in decades to boast an innovative mechanism of action. Approved by the U.S. Food and Drug Administration (FDA) in September 2024, it represents a paradigm shift in the treatment of mental health disorders. Traditional antipsychotic drugs predominantly function by dampening dopamine activity; however, KarXT uniquely targets muscarinic receptors, specifically M1 and M4 subtypes. Research indicates that M4 receptors correlate closely with antipsychotic efficacy while M1 receptors are linked to cognitive processes.
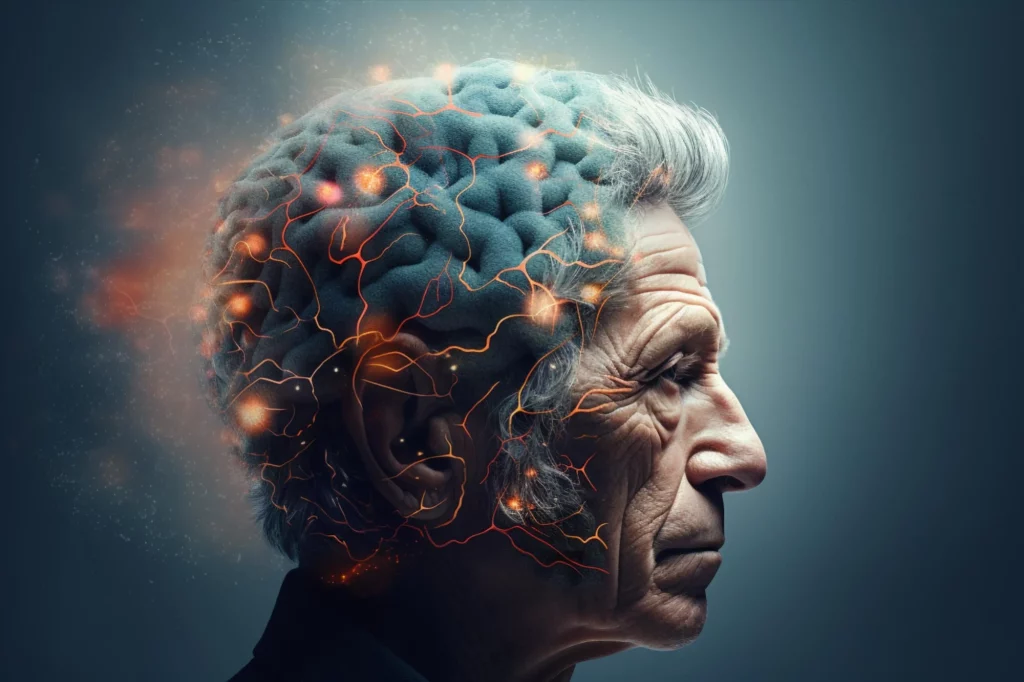
Understanding Alzheimer’s Disease
Alzheimer’s disease is a progressive neurodegenerative condition that insidiously diminishes cognitive function. According to the Alzheimer’s Association, approximately 55 million people worldwide are affected by Alzheimer’s and other dementias. Beyond cognitive decline, patients frequently exhibit psychiatric symptoms such as depression, anxiety, increased aggression, and auditory or visual hallucinations, all of which severely impact their quality of life and that of their caregivers. Notably, no targeted treatments currently exist for the psychiatric symptoms accompanying Alzheimer’s.
Revisiting Xanomeline’s Legacy
The active component of KarXT, xanomeline, was initially developed in the 1990s and shown to alleviate psychotic symptoms in Alzheimer’s patients. However, early clinical trials faced setbacks, as many participants discontinued use due to adverse effects like nausea and vomiting. Consequently, this promising compound was sidelined, alongside similar agents under development. Jeffrey Conn, a pharmacologist at Vanderbilt University, noted that many considered muscarinic agonists a nearly impossible undertaking.
Innovative Combinations for Enhanced Efficacy
Karuna Therapeutics has embarked on a pioneering approach by combining xanomeline with trospium, a compound that blocks muscarinic receptors but does not penetrate the brain, thus mitigating unwanted side effects. This combination, known as KarXT, has shown promise in clinical trials, providing antipsychotic benefits along with cognitive improvements, with fewer side effects than xanomeline alone.
Challenges in Selective Targeting
Despite the potential of muscarinic receptor-targeting drugs, significant challenges remain in selectively targeting specific receptor subtypes due to their structural similarities. Researchers have begun investigating allosteric modulators that bind to non-classical sites on receptors, thereby modifying their functional states for greater specificity. Notably, the drug Emraclidine, aimed at the M4 receptor, was considered one of the most promising candidates in this class but recently failed to demonstrate efficacy over placebo in Phase II trials, highlighting the hurdles in this area of drug development.
Promising Clinical Outcomes
In its Phase II trials concerning Alzheimer’s-related psychosis, KarXT exhibited marked cognitive improvements, with scores approximately 15% higher than those in placebo groups. Furthermore, it was found to reduce psychiatric symptoms by up to 25%. In Phase III trials, over 70% of Alzheimer’s patients reported significant enhancements in mood and anxiety, indicating that KarXT may fundamentally elevate overall quality of life for these individuals.
Exploring Synergistic Treatments
Encouraged by these promising findings, researchers are investigating the potential for synergistic drug combinations. By integrating KarXT with therapies targeting amyloid-beta or tau proteins, its role in comprehensive Alzheimer’s treatment could be considerably amplified.
Real-World Efficacy and Challenges Ahead
While the clinical trial outcomes for KarXT are exhilarating, the real-world efficacy remains to be elucidated. As Carol Tamminga, a neuroscientist at the University of Texas Southwestern Medical Center, articulates, the hospital settings of clinical trials provide tightly controlled environments that do not reflect the complex realities of everyday life, potentially influencing medication adherence and effectiveness.
Future Directions in Treatment and Compliance
In October 2024, Bristol Myers Squibb released findings from a year-long follow-up study focusing on schizophrenia patients treated with KarXT in outpatient settings. While symptoms improved continuously over the year, 11-18% of patients discontinued treatment due to side effects like dry mouth, constipation, and mild nausea—side effects consistent with other muscarinic agents. Addressing these concerns to enhance patient adherence emerges as a crucial challenge.
Optimizing administration methods, such as developing long-acting injectable forms, may reduce daily medication burdens. Additionally, combining cognitive-behavioral therapy with pharmacological treatments could empower patients to manage side effects better, thereby improving overall therapeutic outcomes.
Towards Personalized Medicine
Researchers are also exploring personalized medicine approaches, tailoring drug dosages and treatment plans according to individual genetic profiles, disease progression, and biological markers. This personalized strategy promises to enhance efficacy while minimizing side effects, ultimately improving patient adherence and quality of life.








































Discussion about this post